5 tips to help maximize efficiency in your orthopedic practice
Given the high-stakes nature of orthopedic procedures, it's crucial to run your ortho program as efficiently as possible to avoid delays and cancelations.
At Becker’s Annual Spine & Ortho Conference, a panel of experts agreed that improving the efficiency of surgical care is a key opportunity for independent operators to compete with larger systems. In fact, according to Dr. Andrew Schoenfeld, a member of the panel, the “single most important thing to staying competitive in the market is efficiency.”
Salaries, wages and general/administrative expenses account for almost 40% of ASC operating expenses.1
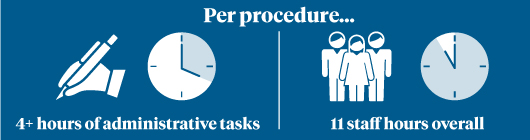 Much of this expense, of course, compensates the talented team of people that helps deliver outstanding patient care every day. Some of these expenses, however, come in the form of wasted time – time spent on administrative tasks and time that could spent on much more valuable things. In fact, over four hours of administrative tasks are needed per procedure, and 11 staff hours overall.1
Much of this expense, of course, compensates the talented team of people that helps deliver outstanding patient care every day. Some of these expenses, however, come in the form of wasted time – time spent on administrative tasks and time that could spent on much more valuable things. In fact, over four hours of administrative tasks are needed per procedure, and 11 staff hours overall.1
Thankfully, there are ways to decrease the administrative burden. Here are 5 tips to help maximize efficiency in your orthopedic practice:
1 | Reduce manual, redundant and paper-based tasks
It can sound easier said than done, but there are tried-and-true solutions to reducing the tasks that keep you from doing more important things.
For example, if you’re ordering your narcotics using the DEA’s paper 222 form, you may want to consider a front-end user interface that automates the task and eliminates the need for paper. Automation systems may be available from your distributor for a nominal fee or no fee at all, and can be accessed from the same system you use to place orders.
Are you manually matching invoices, purchase orders and packing slips? Some online ordering systems allow you to accept and approve invoices online – automating a three-way match with packing slips, purchase orders and invoices electronically and eliminating the need to mail, fax, and scan hard copies of invoices. Check with your supply distributor.
The "single most important thing to staying competitive in the market is efficiency."
2 | Harness the power of kits and trays
According to Dr. James A. Sanfilippo, a fellowship-trained surgeon at Reconstructive Orthopedics in New Jersey, optimizing procedure trays is a great way to manage costs and efficiencies – especially if you're doing bundles.
You’re probably using custom procedure trays (CPT), for your most common cases, but are you taking full advantage of the added efficiency kits and trays can bring? It may be worthwhile to do time studies on some of your less common ortho procedures to assess whether you can save time by pre-kitting them, too.
Many orthopedic practices find that using room turnover kits can help drive consistent and efficient turnover times. By kitting standard items such as sheets and headrest covers with kick buckets and even mops, staff doesn’t need to track down several items after every case.
Ask your supply distributor for a review of your CPTs, kits and trays to assess whether your program is fully optimized.
"Optimizing procedure trays is a great way to manage costs and efficiencies – especially if you're doing bundles."
3 | Use data and analytics
It’s difficult to improve efficiency if you’re not measuring key data that have the biggest impact on your bottom line. In fact, when asked to share insights on running a profitable independent ASC, Alfonso del Granado, compliance officer at Oak Brook Medical Management in Oak Brook, IL emphasized the need to invest in data and analytics to improve efficiencies and grow your margins, adding: “In business as in life, if you’re not growing, you’re dying.”
Accessing key data doesn’t have to cost a lot; in fact, you might already have important metrics at your fingertips and not even know it. This performance dashboard, for example, provides visibility into possible redundancy and waste, and is offered at no charge.
4 | Don't be caught off guard
Procedures such as large joint replacements use a considerable amount of instrumentation, and you don't want to be caught off guard without enough.
In a webcast conversation about how to implement joint replacement services in ambulatory surgery centers (ASC), Dr. Thomas Eickmann stated, "There are also instrumentation considerations. When you get started, there's going to be some sort of capital purchase, and it really has to do with the acuity of cases currently going on at that ASC. It's not uncommon for an ASC to have a sterilizer that only fits two pans at one time, which can make it difficult to do larger volumes of joint replacements. It can be quite onerous to get those sterilized."
Nothing is less efficient than delaying a case due to a lack of instrumentation.
According to Delores O'Connell, senior clinical education specialist with STERIS, obtaining physician preference cards from other facilities is an excellent blueprint for assessing equipment and instrumentation needs for a new joint program. However, she cautions that they may only include general procedural items such as basic orthopedic instrumentation, power equipment, and retractors. In many instances they will not include vendor-specific trays for the joint implants themselves.
"Vendor trays easily add seven to 15 additional large instrument sets to the basic set-up per patient procedure," she adds.
Typically, loaned instrument systems arrive 24-48 hours ahead of the scheduled case. Instrument sets that are delayed by transportation issues or late completion times at the previous facility where used could require overtime to process if arriving less than 24-hours before the scheduled case start time.
"These types of special circumstances may require a second vendor's implant system to be held on stand-by which, can be an additional seven to 15 sets," O'Connell warns.
If a capacity study of washers, sterilizers and ultrasonics hasn't been done, a facility could find they do not have the throughput to process this number of trays effectively and efficiently. Additional planning and processing will need to be addressed if a provider will have more than one case per day. If the capacity of the equipment isn't adequate, this could require hours between cases and may not be the most effective use of surgery suite scheduling or sterile processing operations.
Not all mechanical washers, sterilizers or ultrasonic units are the same. Equipment should be designed to reprocess surgical instrumentation. The manufacturer's instructions for use (IFU) will need to be reviewed for every piece of loaned instrumentation and the equipment called for, as the IFU may contain details that are unique to the devices and may require longer cycles or special handling. Careful planning and right-sizing the equipment to maximize patient care and patient safely can yield a strong ROI on reprocessing equipment.
If you're planning to add a large joint procedure and want to ensure you're prepared, your distributor - working closely with equipment manufacturers' planning experts - can help assess the amount of throughput you'll need based on your expected caseload.
5 | Reduce readmissions
The average rate of readmission 30 days after a hip or knee replacement is 4.2%.2
It goes without saying that readmissions are inefficient, costly and a poor patient experience at best, but do you know the leading causes of readmissions after joint procedures?
From surgical site infections and sepsis, to deep vein thrombosis and fall prevention, there are ways to reduce and even prevent readmissions.
Ask your distributor for more information, or check out our detailed guide for reducing readmissions after a joint replacement.
1: VMG Health Intellimarker Multi-Specialty ASC Study 2017
2: Hospital Compare. Data collected July 1, 2014 - June 30, 2017
© 2021 McKesson Medical-Surgical Inc.